The Iowa 470-0040 form, primarily used for adjustment requests in the Medicaid system, shares similarities with the CMS-1500 form. The CMS-1500 is a standard claim form used by healthcare providers to bill for services rendered. Both documents require detailed patient information, service dates, and specific codes related to diagnoses and procedures. They also necessitate a clear reason for any adjustments or corrections, ensuring that claims are processed accurately and efficiently. This parallel emphasizes the importance of clarity and thoroughness in healthcare billing.
Another document akin to the Iowa 470-0040 is the UB-04 form. This form is utilized by hospitals and other institutional providers to submit claims for services provided to patients. Like the Iowa 470-0040, the UB-04 requires comprehensive details about the patient, the services rendered, and the associated codes. Both forms aim to facilitate proper reimbursement by ensuring that all necessary information is presented clearly to the payer, thus minimizing delays in payment.
The Appeal Request Form is another document that resembles the Iowa 470-0040. When a claim is denied, healthcare providers often use this form to formally appeal the decision. Similar to the adjustment request, it requires a clear explanation of the reasons for the appeal and any additional documentation that supports the claim. Both forms serve the purpose of rectifying issues related to claim processing, ensuring that providers can advocate effectively for their reimbursements.
The Explanation of Benefits (EOB) document also bears similarities to the Iowa 470-0040. An EOB is issued by insurance companies to explain what services were covered, what was denied, and why. When adjustments are necessary, providers reference the EOB to identify discrepancies and submit the Iowa 470-0040 form accordingly. Both documents are integral in the claims process, as they help providers understand payment decisions and guide them in making necessary adjustments.
The Provider Adjustment Request form is another closely related document. This form is specifically designed for healthcare providers to request changes to previously submitted claims. Like the Iowa 470-0040, it requires detailed information about the claim in question and the specific adjustments needed. Both forms are critical for ensuring that providers receive the correct reimbursement for their services and that any errors in billing are promptly addressed.
Additionally, the Claim Reconsideration Request form is similar to the Iowa 470-0040. This document is used when a provider believes a claim was processed incorrectly and seeks a review of that decision. Both forms require a detailed explanation of the issue at hand and supporting documentation to facilitate the review process. They are essential tools for providers to ensure that they receive fair treatment in the claims process.
The Medicaid Provider Enrollment Application also shares some similarities with the Iowa 470-0040. While its primary purpose is to enroll providers in the Medicaid program, it also involves submitting detailed information about services and billing practices. Both documents emphasize the importance of accurate information and compliance with Medicaid requirements, ensuring that providers can effectively navigate the system.
The Health Insurance Claim Form (HICF) is another document that resembles the Iowa 470-0040. This form is used for submitting claims to various health insurance payers. Like the Iowa 470-0040, it requires detailed patient and service information. Both forms aim to ensure that claims are processed smoothly and that providers receive timely payments for their services.
In addition to the various forms discussed, it is essential for Texas residents involved in real estate transactions to utilize appropriate documentation to ensure compliance with state regulations; an important resource for this is the Texas Documents, which provides standardized forms like the Texas Real Estate Sales Contract that outlines essential terms in property sales.
Lastly, the Medical Necessity Documentation form is akin to the Iowa 470-0040 in that it often accompanies adjustment requests. This form is used to justify the medical necessity of services provided, particularly in cases where a claim may be denied. Both documents require a thorough explanation of the services rendered and the reasons for adjustments, underscoring the importance of clear communication in the healthcare billing process.
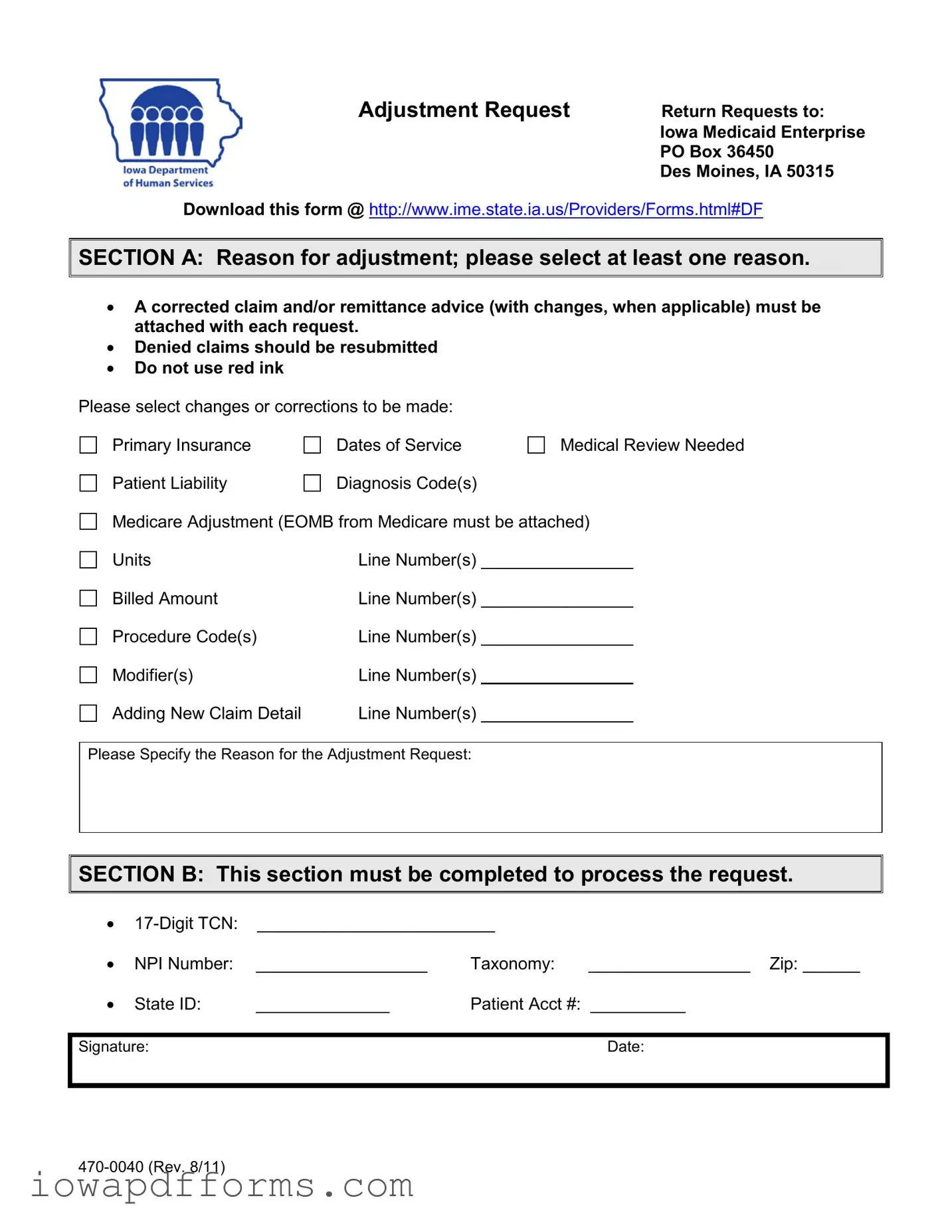


 SECTION A: Reason for adjustment; please select at least one reason.
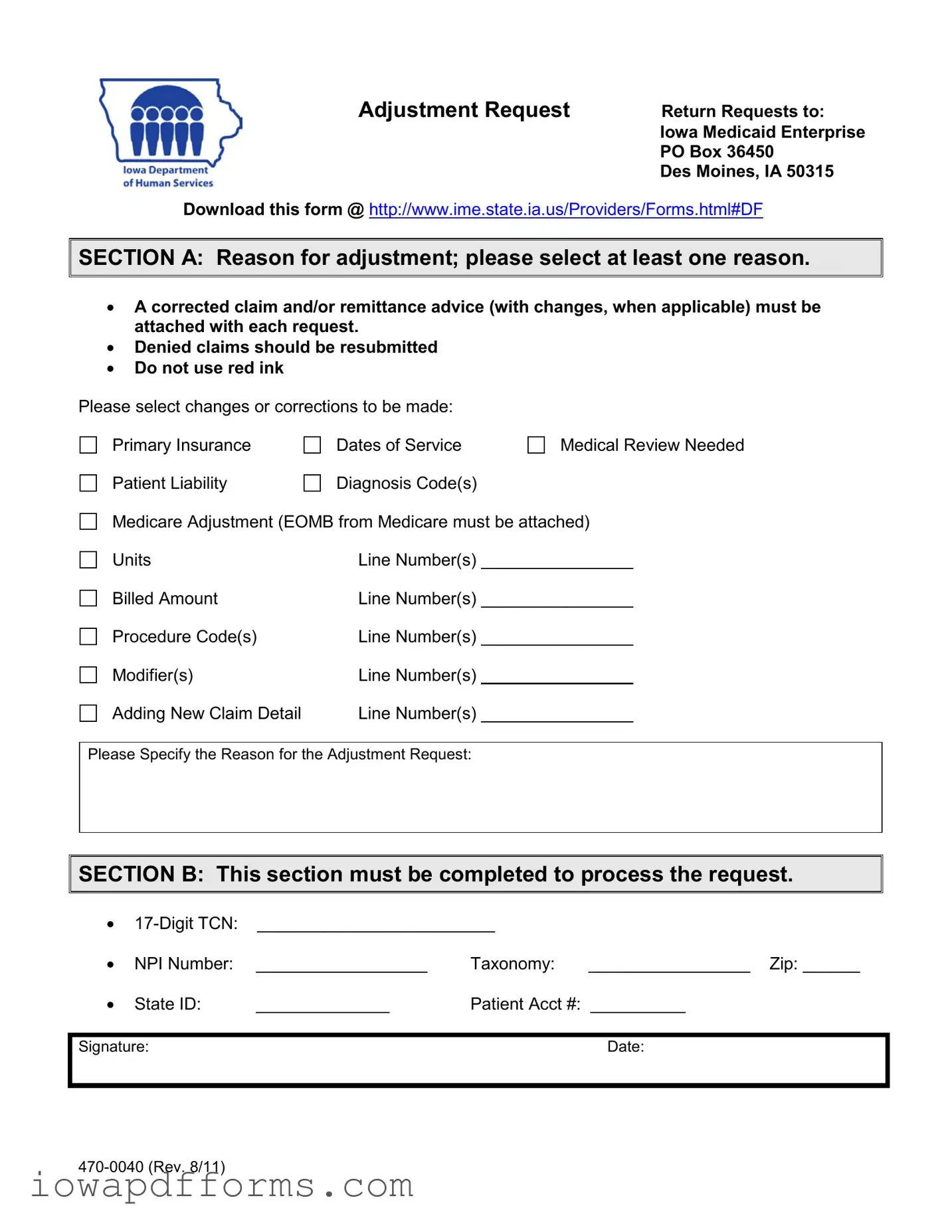
SECTION A: Reason for adjustment; please select at least one reason.

 SECTION B: This section must be completed to process the request.
SECTION B: This section must be completed to process the request.